What is chronic kidney disease?
Chronic kidney disease (CKD) means that your kidneys do not work as well as they should. They can’t remove waste products from your body. Damage to the kidneys' filter system can also allow blood and protein to leak into the urine. This is not always visible but can be found with a urine test.
The term ‘chronic’ means that it is a long-term condition. It does not necessarily mean your kidney damage is severe as many cases of CKD are mild and can be managed with help from your GP and without hospital involvement.
How is CKD diagnosed?
Most people are diagnosed by a blood and urine test. You may have these tests as part of a routine check-up or because you are at risk of developing CKD.
Once you are diagnosed, your doctor will work out what stage of CKD you have. This is done by measuring the amount of creatinine, a waste product that builds up in kidney disease. Your doctors can use this to estimate how well your kidneys are working.
You may hear this referred to as your estimated glomerular filtration rate (e-GFR). It is based on how quickly your kidneys are cleaning your blood and is measured in millilitres per minute.
Most people with CKD stages 1 to 3 can manage the condition themselves with their GP and do not need any specialist input from kidney doctors.
CKD can slowly get worse over time, although for most people it remains stable and only a very small number of people will need renal replacement therapy, such as dialysis. It is unusual for kidney function to improve dramatically once your kidneys have been damaged but it does depend on the cause of the problem.
| Stage of Chronic Kidney Disease | Description | e-GFR Level |
|---|---|---|
One |
Kidney function remains normal but urine findings suggest kidney disease |
90 ml/min or more |
Two |
Slightly reduced kidney function with urine findings suggesting kidney disease |
60 to 89 ml/min |
Three |
Moderately reduced kidney function |
30 to 59 ml/min |
Four |
Severely reduced kidney function |
15 to 29 ml/min |
Five |
Very severe or end-stage kidney failure |
Less than 15 ml/min or on dialysis |
Is CKD common?
Yes. Around 10% of people in the UK have CKD. In people over the age of 80 this increases to 20%. Usually this is mild, and it may not become severe. The vast majority of patients with CKD do not have any symptoms and do not need specialist input.
Who gets CKD?
Anyone can get CKD. It can affect children and adults of any age. Some people are born with it, and some develop it as they get older. It can run in some families and is more common in people from Asian or African backgrounds.
What can increase the risk of developing CKD?
There are lots of causes of CKD. The most common causes include:
- diabetes
- heart disease
- high blood pressure (hypertension)
- inflammation within the kidneys (glomerulonephritis)
- blockages to the flow of urine such as prostate problems or cancers in the bladder
- certain medications such as non-steroidal anti-inflammatory drugs (NSAIDs), which include ibuprofen (Brufen or Nurofen) or diclofenac (Voltarol) among others
- family history of kidney disease, which may include inherited diseases.
Your doctor will try to find out what has caused CKD in your case.
For the majority of people, your GP will look after you, but some people will need to see a kidney specialist and have further tests. It is not always possible to find out what has caused the damage.
What are the symptoms of CKD?
Most people do not have symptoms related to CKD. Even when your kidneys are damaged, they can still work well enough to prevent you having any symptoms. You can be born with just one kidney and remain healthy.
You may still produce normal amounts of urine, even if you have CKD, but your kidneys are unable to remove the toxins from your body that they need to in order to keep you healthy. It is the quality rather than quantity of urine that you produce that matters!
Symptoms may only be noticeable with more advanced kidney disease. These include:
- generally feeling ill, lack of interest in everyday activities and loss of concentration
- tiredness, low energy levels
- muscle weakness
- finding it difficult to breathe (due to a build-up of fluid in the lungs)
- difficulty sleeping at night (insomnia)
- passing urine more often at night
- feeling sick
- headaches
- itching
- aching bones
- muscle cramps.
Why does it matter if I have CKD if I don't have any symptoms?
Although you may not have any symptoms from CKD, kidney damage can still affect your health. CKD can increase your chance of having high blood pressure, heart disease or a stroke. It is therefore important that you are reviewed regularly by either your GP or your kidney doctor.
Having CKD gives you have a higher risk of developing acute kidney injury (AKI). This is a sudden drop in kidney function, often due to an illness or infection. AKI can usually be treated very effectively but it can cause a permanent reduction in your kidney function.
What will my kidney doctor do if I am found to have CKD?
At the first visit, your specialist kidney doctor will try and find out the cause of your CKD. After that visit, each time you go you will have your weight and blood pressure measured and a sample of your urine will be checked for signs of blood, protein or infection.
You will have a blood test to measure your kidney function and check for signs of anaemia, bone health and blood acidity levels. You will then speak to the doctor about your symptoms and discuss which treatments are available.
What will the doctors do then?
- Find out the cause of your CKD and treat it if possible.
- Work with you to make important choices on how to manage your condition.
- Discuss possible lifestyle changes and medication that may relieve symptoms and slow the CKD progression.
- Assess and reduce your risk of heart disease and strokes.
- Try to relieve any symptoms.
- Treat any complications such as anaemia and mineral changes.
What treatment is available?
If your CKD is mild and your kidney function is stable you will normally be referred back to your GP. You should have yearly check-ups to make sure everything is okay but may not need any specific treatment.
You may receive treatment for some of the symptoms of kidney disease, including anaemia and fluid retention, and treatment to keep your bones healthy.
If you are approaching the later stages of CKD, you should start to be given information about the long-term treatments available. These are:
- kidney transplant
- dialysis
- conservative management.
There are big decisions to be made, and support and advice will be given to you by all the professionals in the kidney unit to help you decide what you want to do.
Sign up to receive CKD information by email
By giving us your email address, you're giving us permission to send you the latest news from Kidney Care UK. Further information about how we protect and use your personal data is available in our Privacy Policy. If you would like to change the way we communicate with you at any time please email [email protected]. You can unsubscribe at any time by using the link at the bottom of every email we send.
What can I do to help myself?
- If you smoke, it’s a good idea to try to stop. Ask for help in stopping if you need to. There are lots of treatments to help.
- Try to control your blood pressure. Take any blood pressure medications regularly and as directed by your doctor. Reduce the amount of salt in your diet to less than 6g (one teaspoon) per day. You can find advice on how to reduce your salt intake on the FoodSwitch UK website.
- Take regular exercise. See the exercise section of our website.
- Eat a healthy and balanced diet. You may be able to get support from your GP or dietitian where this is available. You can find out a lot more about following a kidney-friendly diet on our Kidney Kitchen site.
- Maintain a healthy weight. If you are overweight, have diabetes or advanced kidney disease, and need advice on your diet, ask your GP about the services available in your area. They may refer you to a specialist dietitian for advice.
- Avoid non-steroidal anti-inflammatory drugs (NSAIDs). These include common medications like ibuprofen, which can make kidney disease worse. Ask your pharmacist each time you are given a new medicine to check that it is okay for you to take with your reduced kidney function.
If you are unwell you may need to temporarily stop taking certain medications. This is particularly important if you take blood pressure medications. Please discuss this with your GP, pharmacist or kidney specialist.
Do not stop your medication without taking medical advice.
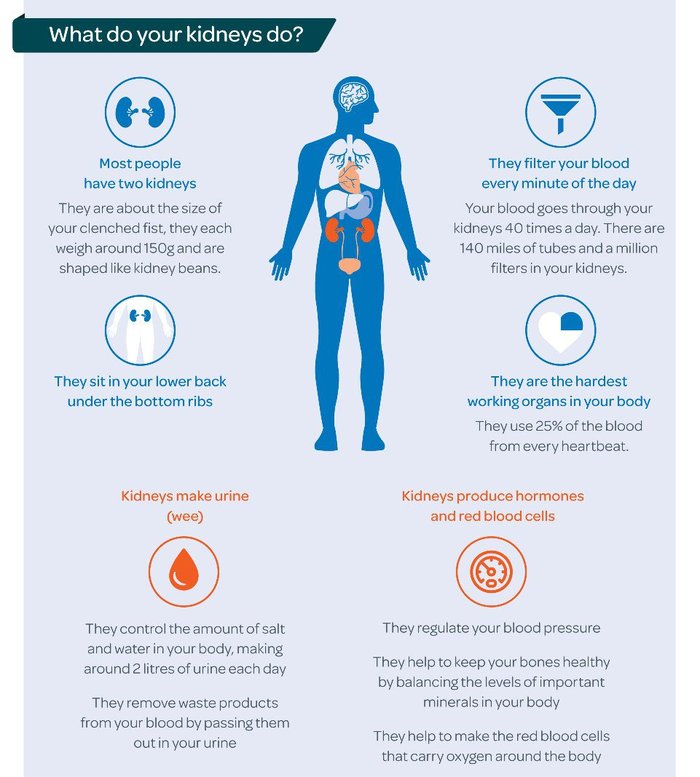
Understanding our kidneys
Most people have two kidneys, although 1 in 10,000 people are born with only one kidney. If we are healthy our two kidneys work by filtering out waste products from the bloodstream, which are passed out of the body as urine.
Our kidneys help to control our blood pressure and they make a hormone that helps create red blood cells and stops anaemia. They also play a very important role in maintaining healthy bones.
In addition, they keep a number of salts and chemicals, such as sodium, potassium, phosphate and calcium, at the right level in the body. Any chemical imbalances can cause problems in other parts of the body, and as kidney disease can interfere with some medications it is important that patients seek advice from their GP or consultant.
Getting support
We know how difficult being diagnosed with a long-term condition like kidney disease can be. We’re here to give support to help improve the quality of life for everyone affected by kidney disease and have a number of ways we can help support you:
- Financial support – If you’re a kidney patient struggling to make ends meet, we may be able to help you.
- Advice and support – Our national Patient Support & Advocacy service provides personal help and support to anyone affected by kidney disease.
- Counselling and support service – Our counselling and support service offers support, information, and guidance.
- If you haven't already signed up to hear the latest news and information from us, you can do so on our sign-up page.
Living with kidney disease
Kidney disease affects different people in different ways, both physically and emotionally. It can impact on many aspects of life, including personal relationships, jobs, and social life.
You can get help with the many aspects of living with kidney disease, including mental health, diet, fluid restrictions, questions to ask your doctor, and benefits, on our living with kidney disease section.
Kidney failure
For most people with chronic kidney disease, there is only a mild or moderate reduction in kidney function with few symptoms. However, it can develop to a more serious stage where the kidneys no longer work. This is called kidney failure.
Around 10% of people with CKD may reach a stage that is known as established renal failure when the kidneys can no longer work well enough to keep us healthy and alive. At this point, your healthcare team will talk to you about dialysis treatment or a kidney transplant.
Remember: it’s never too late to review your choice of care and you can even change your treatment. Always talk to your kidney care team for good advice.
Find out more about kidney failure.

Treatment choices
Kidney transplant – Having a kidney transplant is the best treatment for the majority of patients with established renal failure. Transplantation extends life expectancy, improves quality of life, and offers freedom from dialysis.
Dialysis – Dialysis is a way of artificially removing waste products and unwanted water from your blood. The two ways of having dialysis are:
- Haemodialysis (HD) – where blood is washed through a machine either at home or in hospital as an outpatient.
- Peritoneal dialysis (PD) – where fluid is passed into your abdomen up to four times a day, or overnight at home.
No dialysis – Some patients choose a path called conservative treatment rather than treatment with dialysis. This may suit people with other medical conditions who feel dialysis is not for them.
Find out more about treatments for CKD.
Kidney transplant
This is the most successful treatment for kidney failure. Donated kidneys come from two sources: the national deceased (cadaveric) donor pool, or from a living donor.
Kidneys from living donors offer the best chance of success overall and prevent the need to join the national transplant waiting list. One in three kidney transplants in the UK is now performed from a living donor, either between close family members (blood relatives) or between non-blood relatives, including partners and friends.
It is important to talk about living donation with your friends and family. If you have someone willing to donate a kidney, but they cannot be matched to your blood group and tissue type, there is now a national scheme called ‘paired donation’, which aims to match living kidneys across transplant centres around the UK.
Some units are also developing methods which allow transplantation despite differences in blood groups. Some units can offer treatment to remove antibodies from the blood in order to make an incompatible transplant possible between a donor and recipient.
A kidney transplant before starting dialysis (known as a pre-emptive transplant) is the gold standard of choice, as patients can avoid the need for dialysis altogether and the kidney is likely to last longer.

If you are interested in finding out more about living donation, it is best to talk to a transplant coordinator who will explain the processes and options to you. Donors can also talk in confidence to members of the transplant team before committing to donation.
Not everyone is suitable for renal transplantation, particularly older people and those with other medical conditions. All patients need to have tests to check if they are fit enough to receive a transplant, and some people may need other medical conditions to be treated.
If you are overweight or obese, you may be advised to lose weight before you can receive a kidney transplant.
Haemodialysis (HD)
During haemodialysis, blood flows out of your body and round a dialysis machine, through a dialyser (artificial kidney) that cleans it, and it is then returned to your body. This can be done at home, in a ‘satellite’ haemodialysis unit near your home, or in a dialysis unit in a main hospital.
You will need a small operation to create a ‘fistula’, which is where an artery is joined to a vein, so that the vein can be made bigger to allow dialysis needles to reach your bloodstream. This is usually done six months before you start dialysis, to give it time to enlarge although they can usually be used safely after about six weeks if necessary.
If you need dialysis before a fistula is made, you may have a temporary dialysis line (a small plastic tube) put into a large vein in your neck.
Standard haemodialysis is often for four hours, three times a week on alternate days, but this will vary between patients.
A growing number of patients are now opting for self-care dialysis within the unit as well as home haemodialysis which can offer more independence, either with daily nocturnal dialysis or conventional dialysis, three times weekly at home.
Patients are trained for home haemodialysis by the kidney care team to manage their own treatment, and technical support is always available if it is needed.
Patients who do home haemodialysis insert the dialysis needles into their fistula themselves, or have a spouse, partner or relative trained to do it for them.
Peritoneal dialysis (PD)
This type of dialysis involves putting a small, soft, plastic tube called a catheter into your abdomen (tummy area), which allows dialysis fluid to be drained in and out of what is called your peritoneal cavity.
Waste products are passed from your blood and are absorbed by the dialysis fluid. When the fluid is drained out it takes the waste and extra fluid out of your body.
This can be done either by hand four times a day via a process called continuous ambulatory peritoneal dialysis (CAPD), or by machine overnight and known as automated peritoneal dialysis (APD).
CAPD takes about 20 to 30 minutes to drain the fluid in and out and needs to be done four times a day. APD takes place for eight hours overnight and needs 30 minutes to set up and clean the machine before and after each treatment.
The best way to make a choice about which dialysis treatment will suit you is to talk to the staff and to other patients about what they like and don’t like about their treatment choice. It is usually possible to change your type of dialysis if you want to after some planning.
Choosing not to have treatment
Some patients would rather not have any treatment for their kidney failure. Many units now have a dedicated team of nurses who are able to provide support and care for these patients and their families.
It is important to remember that dialysis and transplantation is not for everyone, and that people have the right to choose not to be treated.
Patients who choose not to have dialysis are usually managed in the same way as other patients with CKD until the point at which the kidney fails. At this point, the priority of care changes to relieving the symptoms of kidney failure and managing its complications.
Information for patients
There are lots of helpful materials that provide information about different types of treatment and its impact on health and lifestyle.
They are available from charities like Kidney Care UK, as well as from your kidney unit and the NHS website.
Some units also have peer support groups where you can speak to other patients who have been through similar experiences.
Order or download patient information leaflets.
Chronic kidney disease: download or order Kidney Care UK's information leaflet
You can download our Chronic kidney disease (CKD) leaflet for free.
You can also order a printed copy of Kidney Care UK’s Chronic kidney disease (CKD) leaflet to be sent to you in the post.